In this post, I focus on the implications of insulin absence/resistance. In other words, the pathophysiology of diabetes mellitus.
There are numerous signs and symptoms to watch for if the condition goes undiagnosed or untreated. I will categorise these as:
- Raised blood glucose levels.
- Tissue degeneration, and immune system / tissue repair dysfunction.
- Increased cardiovascular disease risk.
- Tiredness, hunger and weight loss.
- Fluid balance dysregulation.
Raised blood glucose levels (hyperglycaemia)
Previously I established that insulin helps to reduce blood glucose levels in two ways:
- By facilitating the movement of glucose into cells.
- By facilitating the creation of glycogen.
So, if insulin is absent (or present in insufficient quantities), blood glucose levels will rise. Fasting blood sugar concentrations of more than 7 mmol/L indicate diabetes. However, levels approaching 7 mmol/L indicate a prediabetic state and should be acted on.
Tissue Degeneration, Immune System and Tissue Repair Dysfunction
 Although our body requires a regular supply of glucose in our bloodstream, too much glucose over a period of time can cause a number of problems. High glucose concentrations irritate the inner lining (the endothelium) of blood vessels – both large and small. Let’s start by looking at the effects on capillaries first.
Although our body requires a regular supply of glucose in our bloodstream, too much glucose over a period of time can cause a number of problems. High glucose concentrations irritate the inner lining (the endothelium) of blood vessels – both large and small. Let’s start by looking at the effects on capillaries first.
The picture on the left shows the breakdown of a capillary network in the retina of the eye, with signs of many small haemorrhages and the formation of new capillaries. This is referred to as diabetic retinopathy and can lead to permanent loss of sight if it is not treated. Please bear in mind that if you are working with service users with type 2 diabetes mellitus (DM2) and they have started to experience blurred vision, there may be less serious and more treatable causes.
Another example of capillary degradation can be seen with diabetic nephropathy. This is a condition that has previously affected 1 in 3 individuals who have had diabetes for 20 years or more. It is also one of the leading causes of mortality in individuals with diabetes. The kidney is made up of about 1 million nephrons. As the picture shows, each nephron has a ball of capillaries called a glomerulus. This is where water and waste products are pushed out from the bloodstream to become urine. Over time, high concentrations of glucose lead to a breakdown of the glomerulus. Early symptoms are protein in the urine (proteinuria) but lead to progressive kidney failure, a decrease in glomerular filtration rate, and rising hypertension (as the vascular system struggles to rid itself of fluid).
Capillaries provide oxygen, nutrients, antibodies, growth factors, fluid, and many other substances to tissues around the body. It follows that if these capillaries deteriorate, then it can lead to widespread problems. Issues such as slow wound healing, diabetic neuropathy, and compromised immunity can – at least in part – be attributable to an impaired blood supply. Do any further reading into the pathophysiology here, however, and you’ll quickly discover that hyperglycaemia has a diverse and complex impact on our metabolism – way beyond the scope of this blog post.
Regardless of the complexity of the biology here, it’s vital to recognise that slow wound healing, sensory loss, and compromised immunity are a dangerous mixture of factors, especially when considering mental health service users’ foot care. You will all know what the impact of mental illness is on self-care; 15% of all individuals with diabetes will experience diabetic foot ulcers, and these can quickly lead to lower leg amputations. This risk is understandably higher in individuals with mental illness, as this open-access metanalysis shows.
Before moving on, I mentioned above that diabetic neuropathy can lead to reduced sensation – this is something that is particularly common in our extremities. However, it can also lead to reduced motor function and it can even affect our autonomic nervous system: If the vagus nerve deteriorates, this can cause gastroperesis. This is when food does not pass through the gastrointestinal tract fast enough and it can cause problems such as heartburn, nausea and vomiting.
Cardiovascular Disease Risk
Macrovascular disease (damage to larger blood vessels, like our arteries) accounts for more than 70% of all deaths in service users with DM2 (Gadi & Samaha, 2007). There are some simple connections that can be made here:
First of all, individuals with a diet that is consistently high in sugar and saturated fats are naturally going to have raised cholesterol and triglycerides in their bloodstream. However, this is also one of the risk factors for developing DM2. Secondly, in DM2, due to insulin resistance, the ability of insulin to transport lipids out of the bloodstream is compromised, further raising blood lipid levels and leading to a state of dyslipidemia.
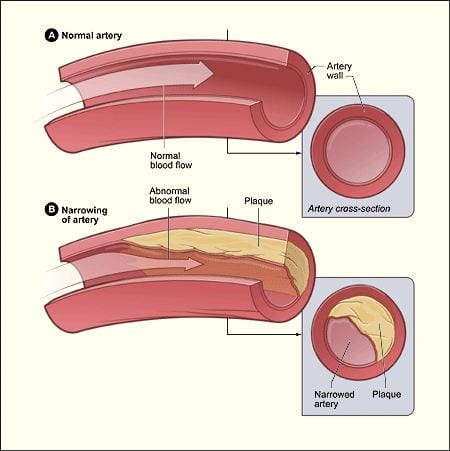
But what happens to those excess lipids in the bloodstream? Do they stick to the artery walls? Not quite -no. Our blood vessels’ endothelium is quite similar to the Teflon coating of non-stick kitchenware. However, if you look particularly closely at the picture on the left, you’ll see that the obstruction to the blood flow is underneath the endothelium. This is what’s referred to as an atherosclerotic plaque. As this video from Osmosis shows, the process of atherosclerosis development is a fairly complex one… so here are the highlights:
- The process is initiated by damage to the endothelium. As we’ve already established, hyperglycaemia does this but so do high levels of LDLs (Low-Density Lipoproteins, or ‘bad cholesterol’), chemicals from smoking, and high blood pressure. Because atherosclerosis also raises blood pressure, this creates something of a vicious cycle.
- LDLs get stuck underneath the damaged endothelium, where they are joined by macrophages, inflammatory cytokines, and smooth muscle cells from the layer beneath.
- The resulting plaque is thrombogenic, meaning that it attracts platelets, and if it is damaged further, it can lead to sudden blood clot formation. This is the basis of life-threatening ischaemic events, like myocardial infarction, pulmonary embolism or ischaemic stroke.
- Plaques cause the arteries to calcify. This hardens them, making them brittle and prone to an aneurysm or haemorrhage.
Tiredness, Hunger and Weight Loss
First a little recap: As the straightforward video from Khan Academy shows, insulin is required to facilitate the movement of glucose into cells. If there is no insulin (as with DM1) or insulin resistance (DM2) then cells are deprived of their primary energy source. We are the product of our 37 trillion cells; if our cells lack energy, then so will we; if our cells are hungry for more, then so will we be. As a backup source of energy, our body can use lipids. When we metabolise lipids, we create compounds called ketones. You may have heard of ketogenic diets – those where carbohydrates are heavily regulated but protein and fat aren’t; the principles are the same. Benefits, as well as risks, have been associated with ketogenic diets, however unregulated ketone production can be potentially life-threatening. Typically it’s individuals with insulin-dependent diabetes who go for protracted periods without enough insulin that are at greatest risk of developing diabetic ketoacidosis. This is why blood sugar machines prompt you to check for ketones with a particularly high reading.
Remember that insulin acts to facilitate the movement of other raw materials from the bloodstream and into cells: lipids to form adipose tissue, amino acids to form proteins like muscle. With an insufficient supply of insulin, this won’t happen as effectively. Therefore less adipose tissue and muscle is made. In addition to this, if the body is utilising adipose and muscle as an alternative energy source to glucose, this can lead to further weight loss. This narrative is made complicated when you consider individuals with DM2; weight loss may be offset by high quantities of sugary and fatty foods. However, what we tend to see is individuals with DM2 gain a significant amount of weight when they are started on particular treatments that increase insulin availability.
Fluid Balance Dysregulation
I’m always a fan of good homemade science experiments! The Sci-guys above brilliantly demonstrate the osmotic force of a highly concentrated sugar solution on an egg, and provide a great little bit of theory at the end… you may have to put up with some corny egg jokes before that though. Principles of osmotic force explain the last of the symptoms discussed in this post.
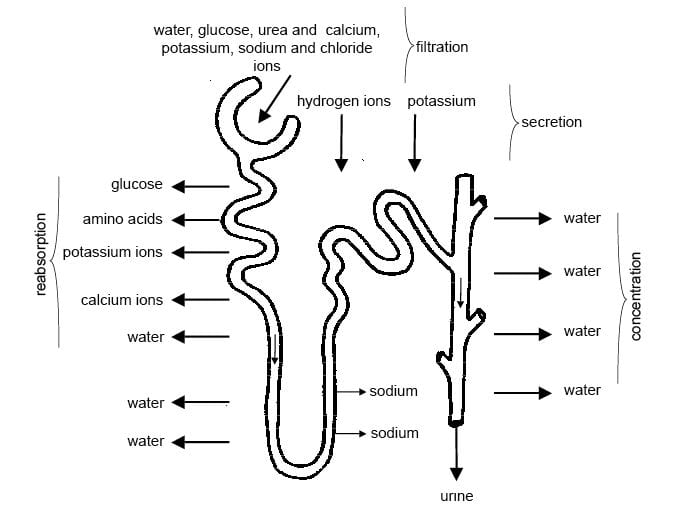 Earlier on, I discussed the nephron. I mentioned that we excrete a few products from the bloodstream via the glomerulus. However, this is just the beginning of the story with urine production. At this stage, the watery content in the nephron is referred to as filtrate. A substantial amount of water is then reabsorbed from the filtrate and back into the bloodstream by the process of osmosis. For people with well-regulated blood glucose levels, any glucose in the filtrate is also quickly reabsorbed back into the bloodstream. In people with diabetes, when glucose concentrations in the filtrate reach significantly high levels, not all the glucose can be reabsorbed. This leads to residual glucose in the urine. Fun fact: Physicians used to look for a sweet taste to urine as a way of diagnosing diabetes mellitus, and the word mellitus actually means honey-like in Latin.
Earlier on, I discussed the nephron. I mentioned that we excrete a few products from the bloodstream via the glomerulus. However, this is just the beginning of the story with urine production. At this stage, the watery content in the nephron is referred to as filtrate. A substantial amount of water is then reabsorbed from the filtrate and back into the bloodstream by the process of osmosis. For people with well-regulated blood glucose levels, any glucose in the filtrate is also quickly reabsorbed back into the bloodstream. In people with diabetes, when glucose concentrations in the filtrate reach significantly high levels, not all the glucose can be reabsorbed. This leads to residual glucose in the urine. Fun fact: Physicians used to look for a sweet taste to urine as a way of diagnosing diabetes mellitus, and the word mellitus actually means honey-like in Latin.
The residual glucose in the filtrate exerts osmotic force. It doesn’t quite draw water into the nephron like the corn syrup did to the egg above… however, it does contribute to less water being reabsorbed into the bloodstream. This has a few knock-on effects. First of all, it means that greater volumes of urine are produced. It also leads to a lower concentration of water in the bloodstream. Together with the high concentration of glucose in the blood, osmotic force is exerted on cells, leading to cellular fluid loss and a sense of thirst. If glucose concentrations are severely dysregulated, this can lead to extreme fluid loss, and pronounced dehydration referred to as a hyperosmolar hyperglycaemic state. This tends to affect people with DM2 more, and it can be life-threatening.
Fluid loss in particular tissues can lead to other common signs and symptoms. For example, blurred vision is frequently the result of dehydration and swelling of the lens.
Further Reading and References:
- Gadi, R. & Samaha, F.F. 2007, “Dyslipidemia in type 2 diabetes mellitus”, Current Diabetes Reports, vol. 7, no. 3, pp. 228-234.
- Nasrallah, H.A et al. 2006, “Low rates of treatment for hypertension, dyslipidemia and diabetes in schizophrenia: Data from the CATIE schizophrenia trial sample at baseline”, Schizophrenia Research, vol. 86, no. 1, pp. 15-22.